Meditation and Prayer - How They Can Help You Live Longer
In an ever-evolving and modernizing world, we often overlook some of the simplest things. Many cultures are based around certain foods and religious values that teach a way of life. In these cultures, practising these religious values creates a sense of community that binds the group together and further emphasizes the culture. But as families move to new cities and countries, holding on to that cultural upbringing that includes religion, becomes harder and harder.
Anxiety, worry and stress exist across cultures and continents. Nobody is immune. However, in North America, the perception of stress appears to be more obvious and our busy lifestyles give us less time for community and culture. Yet those with a strong religious upbringing turn to prayer as a support in coping with stress. Does turning to prayer help moderate the stress response in the body? If so, does that mean individuals who pray regularly have a lower risk of chronic disease, early aging and other stress-related illnesses?
The Stress Response

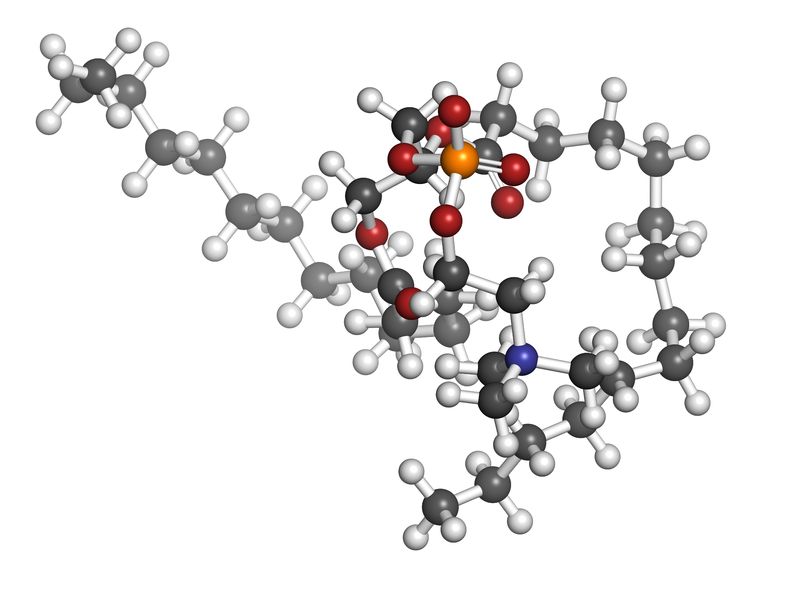
Cortisol is the stress hormone released from the adrenal glands in the human body. It normally rises first thing in the morning to provide enough energy to get started with the day. After this, cortisol should normally fall steadily, until the nightfall when cortisol should be low. At this time, melatonin starts to rise and we feel tired enough to sleep. Melatonin and cortisol work opposite each other. When one is high, the other should be low. If we are not able to manage our stress well or are working late into the night, cortisol levels remain high much longer than they should. This means there is less time to gradually increase your melatonin and quality of sleep will be greatly affected.
Cortisol has effects on almost every aspect of human physiology. It imbalances your blood sugar, increases your risk of insulin resistance and Type 2 Diabetes, and results in stubborn abdominal weight gain. Cortisol depletes our energy, makes us crave unhealthy things late at night and weakens our immune system. The long term effects of high cortisol include high blood pressure, cardiovascular disease and depression. These 3 chronic diseases account for a large percentage of our Canadian medical expenditures, and stress rarely takes the credit for causing them.
High levels of cortisol affect our ability to make connections within the brain. It puts our nervous systems in a constant state of ‘fight or flight’, speeding up our mental processing but not allowing us to focus on any one thing in particular. In a study published in November 2018, evaluation of middle-aged adults using brain MRI showed microstructural changes in the brains of those with high cortisol. These individuals reported worsened memory and visual perception with higher cortisol and this was especially evident in women (1).
A Short History of Prayer and Meditation
Spiritual practices vary across the globe and make it very difficult to objectively measure. Prayer has evolved over time in certain areas, and remained exactly the same in others. Meditation is a form of prayer in certain cultures and has been largely adopted in other cultures as a non-religious activity. It is important to define what “prayer” and “meditation” are, as religious practices can differ. For the purposes of this article, prayer and meditation involve silence and stillness.
The Study of Religion and the Brain

Exactly what prayer does to the human body and brain, has been an interest for scientists and researchers for years. Neurotheology is the term used to describe the scientific study of religious and spiritual beliefs, and their effects on the nervous system. Basically, the connection between religion and the brain. It is a combination of psychology, anthropology, neurology, theology and cognitive neuroscience. Neurotheologists have adapted their techniques in order to assess people of different religious practices.
Dr. Andrew Newberg has been studying neurotheology for over 20 years, performing brain scans while his patients meditate or pray. He finds that the activity in the brain changes when concentrating on the same thing over and over again. There is increased activity of the frontal lobes of the brain, which are largely responsible for attention, behaviour and expressing language. He has found that meditation can improve memory and concentration. People who meditate and pray have reported reductions in anxiety, depression and stress (2). In another study on young Mormons in Utah, a functional MRI scan showed activation of the same reward-processing brain circuits as sexual activity, gambling and taking drugs (2). This study was based on another study, which found elevated levels of serotonin, the happiness hormone, and endorphins during prayer. Participants experienced this as a feeling of peace, warmth and safety.
The Effects of Prayer and Mental Health
Unlike the studies on the brain, studies on mood and mental health are much more subjective. Numerous studies have shown prayer to be a key factor in improving anxiety and depression scores. Indeed, the effects of prayer have been so beneficial for mental health, that researchers have suggested including religious practice in psychiatric care. The existence of religious faith and practice is associated with a meaning in life, greater hope, self-esteem and optimism. The challenge when it comes to psychiatric care, is that the greatest benefit on mental health is seen in those with the strongest religious commitment.
In a study of 330 Christian adults during prayer, the effects of prayer on mental and physical health were correlated with the level of religious commitment. Those with a stronger spiritual connection were more likely to experience reductions in anxiety and depression (3).
Out of 70 cohort studies, 39 showed a greater religious or spiritual connection was linked with the lowest levels of depression. It is important to note that seven out of these studies showed worsening symptoms of depression. Researchers found these individuals had a negative relationship with religion, which included feelings of guilt and disappointment in a higher being (4). Most of the studies done on religion at mental health at this time have focused on Christianity and Christian practices. It will be interesting to note how these results may vary if other religions are taken into account.
The Effects of Prayer on the Stress Response
As mentioned previously, high stress and high cortisol are very real problems within our North American society. Prayer and meditation are effective tools for reducing the amount of cortisol in the blood stream.
A group of medical students had their blood cortisol levels tested before and after a 4-day mindfulness meditation program. Subjective scores of stress had reduced as well as objective measurements of serum cortisol. This study concluded that mindfulness meditation “may decrease the risks of diseases that arise from stress such as psychiatric disorder, peptic ulcer and migraine” (5).
When cortisol is lowered, the nervous system calms down and decreases the fight or flight response. When rapid-fire thought processing slows down, other symptoms of anxiety subside within minutes. On a physical level, heart rate returns to the normal range, blood pressure decreases and breathing becomes deeper and slower.
Because cortisol creates inflammation in the brain, this toxic environment is a perfect breeding ground for worsening anxiety. In the body, inflammation can show up in the joints as arthritis, skin as eczema, and digestive tract as indigestion. Inflammation can be measured as elevated levels of signalling molecules IL-6 and TNF-a. In any situation of stress, including exams, presentations or chronic illness, levels of inflammatory cells increase in the body. If meditation has the potential to lower inflammation in the brain and reduce anxiety, there is potential for it to improve symptoms of inflammation in the rest of the body as well. Studies up to date have reported improvements in self-reported levels of stress after meditation. However, there is no objective data to suggest that meditation lowers these inflammatory markers in the body.
Prayer As An Effective Tool
Prayer and meditation have been around for centuries and have been a basis of cultural and community events. Mindfulness meditation has gained popularity in the workplace because of its effectiveness at lowering self-reported stress and increasing workplace productivity. On a scientific level, prayer and religious practices increase the activity of certain parts of the brain, specifically the prefrontal cortex. Prayer has the ability to increase endorphins, which give us a positive sense of well-being. From a religious standpoint, prayer has been shown to lower anxiety and depression scores, but the greatest benefit was found in those with the strongest religious commitment.
Neurotheology is a fascinating topic of research and one that will likely never provide a clear answer. Could the success of prayer be attributed to the silence and stillness? Or is it the belief in a higher being that makes prayer effective? As religious practices around the world are so different, many questions still remain.
References:
1. Echouffo-Tcheugui, J. et al. (2018) Circulating Cortisol and cognitive and structural brain measures. The Framingham Heart Study. American Academy of Neurology. Retrieved from: https://n.neurology.org/content/91/21/e1961
2. Blumberg, Lynne. (2014) What happens to the brain during spiritual experiences? The Atlantic. Health. Retrieved from: https://www.theatlantic.com/health/archive/2014/06/what-happens-to-brains-during-spiritual-experiences/361882/
3. Jeppsen, B. (2015) Closeness and control: Exploring the relationship between prayer and mental health. https://doi.org/10.1002/cvj.12012
4. Dein, Simon. (2018). Against the stream: religion and mental health – the case for the inclusion of religion and spirituality into psychiatric care. BJPsych Bull. 2018 Jun; 42(3): 127–129.doi: 10.1192/bjb.2017.13
5. Turakitwanakan, W et al. (2013). Effects of mindfulness meditation on serum cortisol in medical students. J Med Assoc Thai. 2013 Jan;96 Suppl 1:S90-5.