Concussion Management - Long-Term Consequences of Repeated Brain Trauma
As Canadians, athletes are our celebrities. They win us championships and gain us worldwide recognition. They put our cities on the map and encourage future generations to continue their success. Because the retirement age for most sports is fairly young, we rarely hear about our celebrity athletes after they leave their sport. Hockey players, football players and boxers all sustain tremendous amounts of head trauma over their career. Repetitive brain injury creates lasting effects on their physical and mental health, which we rarely hear about on the news.
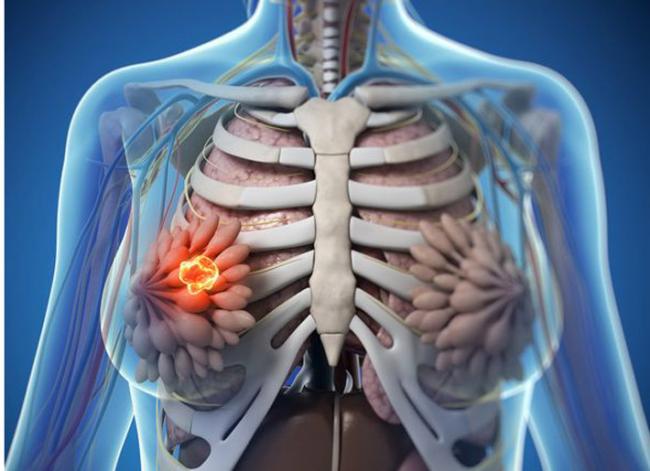
The brain is a vital organ surrounded by numerous layers of protection within our skull. The nutrient-dense cerebrospinal fluid (CSF) bathes the brain and cushions it against the walls of the skull. For most movements of the head, the CSF protects the brain from injury. When an individual sustains head trauma, the brain rattles within the skull and can create an altered mental state. Depending on the intensity of the trauma, the injury can include bleeding in the brain, loss of consciousness and skull fracture.

Concussion is one of the many terms that falls under the umbrella of Traumatic Brain Injury (TBI). These other terms may include contusion, second impact syndrome and penetrating injury. At the end of the day, the treatment for all forms of TBI is exactly the same.
In the moment, signs of a TBI can include headaches, loss of consciousness, ringing in the ears, dizziness and vomiting (1). This may warrant a visit to the hospital or doctor’s office. However, medical doctors are very limited in their management of head trauma. The current concussion guidelines suggest that rest, anti-inflammatories and avoidance of screen time are the best tools.
After a few weeks, the initial symptoms may have improved, but a vast array of symptoms can arise that are known as post-concussion syndrome. At this point, a patient may feel irritable, depressed, anxious, fatigued or sensitive to light (1). They may have trouble thinking, focusing and sleeping at night. Post-concussion syndrome can last for weeks or years and largely depends on the resilience of the person and the area of the brain affected. A small percentage of patients will be referred to a neurologist who will follow their progress with brain imaging. However the bulk of this patient base is given the diagnosis of post-concussion syndrome and sent on their way.
What Brain Imaging Shows
The best way to investigate TBI is through brain CT and MRI. Brain CT’s are important for diagnosing skull fractures, focal brain injuries and intracerebral bleeding (2). They are not detailed enough to show small injuries that are common with mild TBI. These smaller injuries are often the ones that take longer to repair and produce more clinically significant symptoms. Brain MRI’s have become much more sensitive over time and are able to detect microbleeds within fragile brain structure (1). MRI’s are great for research purposes, however the availability in the clinical setting renders them less useful. In some parts of the country, a wait for an MRI can be months.
Are blood tests useful? Blood testing can be useful for determining the downstream effects of concussion but are less relevant in the diagnosis. Because fragile organs such as the hypothalamus and pituitary gland sit in the brain, they can alter hormone levels in the body if they are damaged. Blood work will often show hormone abnormalities shortly after concussion and will normalize within 3 months. If there is sustained injury to these endocrine glands, hormone therapy may be implemented to mitigate these effects.
Managing Recovery
Over the last few decades, more and more research has surfaced questioning the current concussion management protocol. After a mild traumatic brain injury, an athlete is often asked to rest and restrict exercise. In a few weeks, they are given a steady return-to-play guideline to follow and are often cleared to return within a month. Nowadays, more and more athletes are being asked to skip the rest and perform light cardiovascular exercise, such as walking for 1-2 hours per day within 24 hours after injury. They are told to wear a pair of dark sunglasses to decrease light exposure and stay away from screens. Athletes are show to recover faster this way because instead of resting, we are increasing circulation to the brain and allowing damaged cells to be carried away. With circulation come all the nutrients we need to heal, and this further supports the brain.
Designing a return-to-play program is very important and must include input from all members of the sports rehab team. The lingering cognitive impairments can include processing speed, memory, attention and awareness. For a hockey player, lacking these crucial skills after a concussion can lead to a second hit and more impactful concussion if they return to play too early. The same way muscles require amino acids to repair after a workout, the brain requires essential fats and other key nutrients to repair after injury. The nutritional support at the onset of concussion is such an important step in brain repair and can definitely reduce many of the post-concussion symptoms if implemented immediately. High doses of omega-3 fatty acids can rebuild the brain tissue and reduce the inflammation from the injury. Vitamin D is an important nutrient for cognitive function and has been linked to a reduction in Alzheimer’s disease risk. Vitamin B12 is a key step in the formation of myelin sheath, the protective layer around nerves. Without this, nerve repair may be compromised and show up as poor memory, focus and concentration. Cognitive rehabilitation must fit into a physical rehabilitation program. This includes many of the puzzles and tests used for monitoring Alzheimer’s and dementia patients. They help to strengthen the nerve connections in the brain and improve processing speed. Even once an athlete has returned to play, continuing with these tests for the next few months will further support cognitive function.
Risk of Not Doing Anything
Many athletes will suffer minor concussions and never end up going to the doctor. Many may not experience any symptoms and be ready to play again within a week. More severe concussions create lasting changes in brain structure, which are susceptible to further injury. It is often these second impacts (called second impact syndrome), which are significantly worse and can put an athlete out for months. There is also a risk of brain bleeding after a second injury which can be fatal. After a series of concussions in a short period of time, an athlete must make an important decision as to whether or not the risks of playing the sport outweigh the benefits.
Long Term Consequences of Repetitive Brain Trauma
The long term effects of repetitive brain trauma have been known and studied for decades. Many retired athletes suffer tremendous amounts of mental illness and dementia in their mid-life. Some have even commit suicide, but never make the newspaper headlines. The movie “Concussion” in 2015 highlighted the tremendous influence the NHL, NFL and other major sports leagues had to “hush up” the scientific evidence linking traumatic brain injury to these devastating diseases. The term Chronic Traumatic Encephalopathy (CTE) was used to describe ongoing brain inflammation as a result of repetitive trauma. Since this movie was released, research studies unveiled the long-term effects of sports-related concussion. Major league sports have been forced to make changes to protect their athletes and are monitored by a 3rd party for concussion management of their players (3).
A systematic review of 3819 studies of former athletes showed a positive correlation with number of concussions and severity of depression scores. Only two studies evaluated the risk of suicidal ideation. The authors concluded that repetitive brain trauma and an increased risk of neurodegenerative disease was inconclusive. However it was clear that neuroimaging studies had shown changes to the structure and neurochemical balance in the brain after repeated trauma (4).
On a recreational level, medical professionals are starting to have conversations with patients about sports retirement. The American Academy of Neurology released a practical guide for practitioners to help in their discussions of medical retirement from sports (5). The review highlighted 10 athletes under the ages of 35 and their battle with repetitive head trauma. The guide encouraged practitioners to consider not only the clinical and radiographic evidence of injury, but the athlete itself. Many athletes play high-level sports because of pressure from other coaches and parents, financial motivations, and strongly identify themselves with a sport. Removing someone from a social network built entirely around a sport is not to be taken lightly.
Conversations about medical retirement must include a discussion on the long term risks and the significant impact they can have to academic performance, career success and healthy aging. Providing MRI imaging can prove to be a helpful visual for athletes who have sustained a series of concussions. By opening up this conversation, the athlete may become more aware of the effects of the lasting concussion symptoms and make a decision for themselves.
The brain is an incredible organ with powerful functions, but unfortunately has limited potential to regenerate from severe damage. Making important decisions about sports from an early age is a difficult but crucial step in supporting a healthy life and strong retirement.
References:
- Sharp, D. Jenkins, P. (2015) Concussion is confusing us all. Practical Neurology. 2015 Jun; 15(3): 172–186. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4453625/
- Romeu-Mejia, R. et al. (2019) Concussion Pathophysiology and Injury Biomechanics. Current Reviews in Musculoskeletal Medicine. 2019 Jun; 12(2): 105–116.C. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6542913/
- NHL.com. NHL updates concussion protocol (2016). https://www.nhl.com/news/nhl-updates-concussion-protocol/c-282571624
- Manley, G. et al. (2017) A systematic review of potential long-term effects of sports-related concussion. British Journal of Sports Medicine. Vol51, Issue12. Retrieved from: https://bjsm.bmj.com/content/51/12/969.full
- Davis-Hayes, C. et al. (2018). Medical retirement from sports after concussions. Neurology Clinical Practice. 2018 Feb; 8(1): 40–47. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5839677/